Singapore Government releases White Paper on Healthier SG on 21 September 2022
By Joyce Teo, Senior Health Correspondent, The Straits Times, 21 Sep 2022
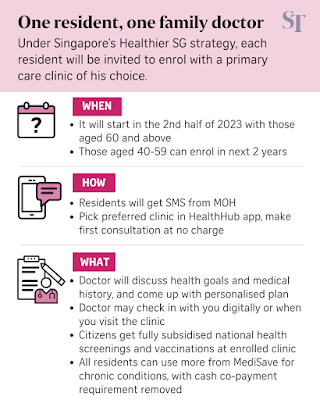
Singapore's ambitious plan to have one family physician and one health plan for each and every one of its residents will start with those aged 60 and above in the second half of 2023.
The Healthier SG Programme will also offer cheaper drugs for chronic diseases at general practitioner (GP) clinics, among other benefits. With it, MOH aims to shift its focus from "sick care" to preventive care so as to eventually help every resident stay on the path to better health.
Eligible residents will be invited to enrol in the programme with a primary care clinic of their choice via SMS. Those in the 40 to 59 age group will be invited to enrol in the following two years, the Ministry of Health (MOH) said in a White Paper that was submitted to Parliament on Wednesday. The White Paper will be debated in Parliament in October.
Since March, the ministry has engaged more than 6,000 residents and other stakeholders for their views on the strategy.
Under the Healthier SG Programme, residents will develop a relationship with a primary care doctor who will holistically manage their health.
At the first visit, which will be free, the doctor will work out a health plan that can include diet adjustments, an exercise regimen and regular health screenings and vaccinations.
Health Minister Ong Ye Kung told the media at the MOH headquarters in College Road on Wednesday that the plan has social prescriptions like "how you eat, how you sleep, how you cut down on salt and sugar, quit smoking, exercise, so on and so forth".
Community partners will be roped in to help manage residents' health, as the idea is to move healthcare away from acute hospitals to the community to help keep people healthy. Residents will be able to join free programmes to keep fit, for instance.
A key change that MOH will introduce to get residents on the programme is to make drug prices at participating GP clinics more comparable with those at polyclinics through a combination of enhanced drug subsidies and drug price limits. This will be done for drugs used to manage common chronic diseases.
With this, people will no longer have to end their relationship with their long-time GPs when they develop diabetes or hypertension just because the drugs for these conditions are cheaper at polyclinics.
MOH will announce the details for this at a later date.
The ministry also said that it will fully subsidise nationally recommended screenings and vaccinations for Singapore citizens, and waive the need for residents to co-pay 15 per cent of their bills in cash when using MediSave for the treatment of common chronic conditions under the Chronic Disease Management Programme.
"We are shifting away from co-payment for this basic preventive care to fully support residents (in) preventive care," said Mr Ong.
There will be a health points reward system to get people to take action, such as to enrol and complete their first consultation, and engage in health activities.
However, to get Healthier SG off the ground, MOH will first have to mobilise family doctors in private practice.
MOH will offer GPs an annual service fee for each enrolled resident, which will vary according to the risk profile, scope of care and the progress made, as well as a tech support grant.
These doctors will need to join a so-called Primary Care Network, partner a healthcare cluster, and be digitally enabled. The Primary Care Networks, which hire nurses and coordinators for chronic disease management and other shared tasks, will support the GPs in their work. There are currently 23 polyclinics and about 1,800 GP clinics, of which 670 clinics have formed such networks.
To ensure the level of care is consistent across GPs, MOH is developing a set of care protocols with primary care leaders to guide family doctors on how to manage key chronic conditions.
Healthier SG will start with the care protocols of three of the most common chronic conditions: diabetes, hypertension and lipid disorders. In the future, the protocols will expand to cover more conditions and areas such as mental health.
"Everyone involved, including healthcare providers, the Government and residents, will need to do things differently," MOH said in the White Paper.
"Healthier SG is probably the most significant change to the health system since Independence. We have had six decades where we emphasised reactive sick care rather than health promotion," said Associate Professor Jeremy Lim, director of the Leadership Institute for Global Health Transformation at the National University of Singapore's Saw Swee Hock School of Public Health.
The incentives under Healthier SG are created to promote health, rather than healthcare and, for the residents, inertia will be the biggest enemy, he said.
It will take years for such a major transformation of the healthcare system to take off and experts said the start will inevitably be challenging before the results show.
"Healthcare expenditure may rise initially and even more rapidly as we discover more people who have medical problems," said Dr Wong Chiang Yin, a public health specialist in the private sector.
"We must have the tenacity to stomach this and stay the course before the benefits of Healthier SG kick in at a later stage," he added.
The White Paper on Healthier SG can be viewed at www.healthiersg.gov.sg.
Additional reporting by Lee Li Ying
How will being paired with a GP under the Healthier SG programme benefit me?
By Lee Li Ying, The Straits Times, 21 Sep 2022
From the second half of 2023, residents aged 60 and above will be able to discuss their health goals and medical history with a dedicated family physician when they enrol in the Healthier SG programme.
The programme will be extended to those in the 40 to 59 age group in the following two years.
This comes as Singapore strives to shift its healthcare model towards preventing individuals from falling ill, instead of reactively caring for those who are already sick.
Since March 2022, the Ministry of Health (MOH) has consulted more than 6,000 residents and stakeholders such as general practitioners (GPs), employers and community partners.
A White Paper on Healthier SG – listing the key features and recommendations of the programme – was submitted to Parliament on Wednesday, and will be debated in October.
The Straits Times looks at how the programme aims to prevent or delay the onset of chronic diseases and ill health.
Q: What can residents expect when they enrol in the Healthier SG programme?
A: When enrolment starts, MOH will send eligible residents an SMS text message to invite them to choose their preferred clinics. During the first consultation, which will be free, the doctor will assess the resident's medical history, health needs and concerns.
For those with no chronic conditions, the doctor will advise them on appropriate preventive measures, such as health screenings and vaccinations, and the Government will fully subsidise the nationally recommended ones.
For those with chronic conditions, the doctor will work with them on follow-up management.
Everyone enrolled in the programme will have a personalised health plan.
To monitor a resident's progress, the GP will check on him remotely, such as over the phone, or when he sees the doctor for other checks. This brief annual check will be subsidised by the Government.
Those with chronic conditions would likely require two to four follow-up consultations annually, and prevailing subsidies will apply for their visits and treatments.
Q: What does a health plan look like?
A: A health plan is an overview of the resident's key health parameters, which include a set of health goals, such as weight loss or improvement in chronic conditions.
The plan would also include follow-ups such as health screenings, diet adjustments and an exercise regimen.
The conversation between the doctor and patient on the desired health outcomes, action plans and care preferences will be based on the health plan.
Q: How can I be sure the level of care is consistent given that different family doctors may have different approaches?
A: To ensure a consistent level of care, MOH is developing 12 care protocols on managing key chronic conditions.
For a start, the care protocols will cover three of the most common chronic conditions: diabetes, hypertension and lipid disorders.
The protocols will lay out recommended health screenings, medication, lifestyle adjustments and when specialist attention or acute care is required.
About a year after the initial launch, MOH will broaden care protocols to cover other common chronic conditions as well as specific screenings required for seniors.
Subsequently, the Government will progressively cover other complex chronic conditions, such as mental health and end-of-life care.
Q: Will all GP clinics be on board this scheme?
A: To participate in the Healthier SG programme, clinics will have to meet a few criteria.
Each GP clinic must have at least one family doctor registered as a family physician within seven years of the launch of the programme's enrolment.
Family doctors must also participate in core government schemes, such as the Chronic Disease Management Programme, Community Health Assist Scheme, and the Screen for Life and national vaccination programmes.
Other requirements include partnering a healthcare cluster and using a compatible clinic management system within a year of the programme's launch.
Q: Will I be allowed to switch doctors?
A: In the first two years after the initial enrolment, residents will be allowed to switch doctors up to four times. This allows residents more time to find a clinic they are comfortable with.
After that, MOH will allow one change a year to accommodate personal preferences and change in life circumstances, such as families who move house.
Q: What about those with employer medical benefits?
A: The Government is urging employers to encourage their panel doctors to participate in the Healthier SG programme so their employees can see the same doctor to enjoy both employer and Healthier SG benefits.
Alternatively, residents can still choose to see a company panel doctor for episodic care, while enrolling with a family doctor for preventive and chronic consultations.
Q: What other incentives are there to encourage residents to lead healthier lifestyles?
A: Today, under the National Steps Challenge by the Health Promotion Board, residents who are active can earn health points, which can be used to exchange for vouchers from merchants such as supermarket chain FairPrice. Residents need to download the Healthy 365 app to accumulate points.
To encourage residents to exercise more, MOH will enhance health points for those on the programme. Beyond just counting of steps, health points will also be awarded for a range of physical activities and even for adherence to diet plans. Details of these are not available yet.
* Parliament: Singapore to spend more than $1 billion to get Healthier SG preventive care strategy up and running
By Joyce Teo, Senior Health Correspondent, The Straits Times, 4 Oct 2022
To get the new preventive care strategy Healthier SG off the ground and running, Singapore will spend more than $1 billion over the next three to four years in set-up costs, such as new IT systems and support to get general practitioner (GP) clinics ready for the scheme.
It will also spend an estimated $400 million a year on recurrent costs, such as annual health screenings for residents and the annual service fee for GPs, Health Minister Ong Ye Kung told Parliament on Tuesday.
"We spend about 6 per cent of our healthcare budget on preventive care annually, such as to fund HPB," he said, referring to the Health Promotion Board.
"With Healthier SG in the coming few years, we will, and we want to, grow this – perhaps to double the share of total healthcare spending," he said.
In making these investments, the primary motivation is to reduce the burden of disease and the suffering of people and their loved ones, he added.
Mr Ong was speaking at the start of the debate on the White Paper on Healthier SG, which outlines a major shift in the healthcare system and was published on Sept 21 after six months of consultations with more than 6,000 residents, GPs, employers and others.
Healthier SG seeks to shift the gravity of care from the hospitals to the community.
The aim is to get residents to build a long-term relationship with one family doctor, who will help them to take charge of their own health and wellness.
In his speech, Mr Ong acknowledged that these investments in preventive care will take time to produce results.
Any impact in people's health will not happen immediately, but perhaps be discernible eight or 10 years down the road.
And with an ageing population, reversing the rise in healthcare spending will not be possible. "What we can hope for is to slow down the rate of increase," Mr Ong said.
Singapore's total healthcare spending could rise by up to threefold in the coming 10 years to about $60 billion a year by 2030, from about $22 billion a year at present, he noted.
"If this national medical bill doubles instead of triples in 10 years – we would have saved much more than what we are planning to spend on preventive care," he said.
"At the heart of Healthier SG is a philosophy of how we choose to live our lives. If we put in a small effort every day, a bit of discipline every week, a bit of restraint every week, we can avoid big life-changing suffering later."
Mr Ong said: "We are making a big effort to support you because it is almost human instinct to not do the right thing because of instant gratification."
Under Healthier SG, once residents sign up with a family doctor, the Government will fully fund the annual check-ins with doctors and nationally recommended health screenings and vaccinations for residents.
The screenings will include common chronic conditions such as Type 2 diabetes, hypertension and hyperlipidaemia, as well as for breast, cervical and colorectal cancers.
Those using MediSave to treat chronic illnesses will no longer be required to co-pay 15 per cent of the bill using cash, and can fully use their MediSave. Subsidies for common chronic disease drugs at private GPs will also be enhanced.
For this to happen, the support of family doctors is key.
"GPs will continue to attend to their existing patients and prescribe medication to them. What Healthier SG does is to enlarge their client pool, through enrolment for preventive and chronic care consultations," said Mr Ong.
The GPs will be paid an annual standard fee per enrolled patient, for maintaining a long-term relationship with him or her.
This fee will cover regular doctor consultations, ensuring residents adhere to their health plans, the associated administrative work and a review of the health plan annually – over and above subsidies for health screenings and medication, which are separately funded, added Mr Ong.
The minister said it is not a new concept for GPs, as those who assist the healthcare clusters to manage complex chronic patients get a "Care Plus" service fee payment of $100 per patient.
"Healthier SG will broaden such schemes to cover preventive care for large segments of the population. The fee will be similar or higher than the current Care Plus fee, depending on the health conditions of the enrolled residents," said Mr Ong.
"We estimate that in the coming few years, Healthier SG service fees and revenue from subsidised services can grow as more residents enrol and become a significant component of a GP's annual revenue – maybe a quarter, maybe a third."
A total of 28 MPs had indicated that they plan to speak during the debate on the White Paper.
Among the 18 MPs who spoke on Tuesday, Dr Tan Wu Meng (Jurong GRC) highlighted the need to look into the challenges faced by those who are not digitally savvy and those who are less mobile, and said that holistic care takes time.
Ms He Ting Ru (Sengkang GRC) asked about the support for GPs, including training in handling mental health cases, and if the barriers for foreign-trained Singaporean doctors to come home to practise can be lowered.
MPs unanimously endorse White Paper on Singapore's healthcare reform plan
24,000 more nurses, healthcare staff needed by 2030 as Singapore ages
By Joyce Teo, Senior Health Correspondent, The Straits Times, 5 Oct 2022
With the number of elderly Singaporeans on the rise, a system to care for the aged is set to become a critical part of the nation's healthcare landscape.
The new initiative to prevent illnesses and keep the citizens healthy is a move in that direction, Health Minister Ong Ye Kung told Parliament on Wednesday.
One key challenge is to find enough foreign nurses to supplement local ones to care for the elderly.
Mr Ong said nurses, allied health professionals and support care staff are needed to operate hospitals, clinics and also eldercare centres.
"They number 58,000 now and MOH (Ministry of Health) estimates that this will need to grow to 82,000 by 2030," he added.
He also pointed out that by 2030, one in four Singaporeans will be aged 65 and above, up from one in six today.
In his closing speech on the debate on the Healthier SG White Paper in Parliament, Mr Ong underlined the need to prepare for a rapidly ageing population from a healthcare perspective and also the urgency to attract foreign nurses, who are in high demand globally but are also critical in making the aged care system work.
He said Singapore's healthcare system is not one system but three interconnected systems working together to deliver good health.
The first is the acute care system, comprising hospitals and emergency departments, where people were treated when they get very sick.
Then there is the public health system, which includes the control of infectious diseases such as Covid-19, as well as population health, which is being beefed up through Healthier SG.
The third one is the aged care system, which is not just about nursing homes, which continue to be built, but also enabling seniors to age in the community.
"In our Asian culture, we value caring for our seniors at home. Our seniors also prefer to age in a familiar environment. We should not lose this," said Mr Ong.
"As a society, we must guard against the assumption that seniors will always become sick and frail, and unable to take care of themselves."
An estimated 97 per cent of seniors above 65 can either live independently or with some help in the community today.
Mr Ong also alluded to research showing that the health impact of loneliness for a senior is the equivalent of smoking 15 cigarettes a day.
"We must maintain or improve that share, and not inadvertently give them that equivalent of 15 cigarettes a day, and weaken their health and ability to live independently," he said.
But he also pointed out that an expanding aged population needs more healthcare. And since there simply are not enough local nurses available for this, Singapore will have to rely on more foreign nurses.
Replying to several MPs, including Ms Mariam Jaafar (Sembawang) and Mr Dennis Tan (Hougang), who had raised issues on manpower, Mr Ong said there has been no exodus of local nurses, and that efforts are afoot to raise the intake of nursing students locally to 2,300, from 2,100 currently.
While locals will continue to form the bulk of the nursing workforce, the number and role of foreign nurses will grow.
"If we want to take care of our seniors and the sick, if we want to reduce the workload of healthcare workers, we must expect foreign healthcare workers to play a bigger role in the coming years," said Mr Ong.
"This is especially so in areas that are facing a bigger manpower crunch, like aged care or palliative care."
In response to Nominated MP and breast surgeon Tan Yia Swam's suggestion of granting permanent residency to the good performers, given the heightened international competition for nurses, Mr Ong said MOH is supportive of this.
The Immigration and Checkpoints Authority assesses permanent residency applications holistically and will certainly consider the important contributions of healthcare workers, and MOH's support for foreign healthcare workers, when evaluating their applications, he said.
Singaporeans and permanent residents make up about 72 per cent of Singapore's pool of registered nurses and 63 per cent of enrolled nurses. The rest are from the Philippines, Malaysia. China, India, Myanmar and other countries.
Mr Ong said MOH will broaden training for existing nurses, allied health professionals and pharmacists so that they can take on crucial roles alongside doctors.
For example, community nurses will be trained in lifestyle coaching to help residents make good choices according to their care needs, he said.
There are also plans to train community pharmacists, who can already provide smoking cessation and weight management services, in influenza vaccination.
"But first, there must be enough people to train," he said,
Meanwhile, Dr Janil Puthucheary, Senior Minister of State for Health, in his reply to Mr Xie Yao Quan (Jurong) and Ms He Ting Ru (Sengkang), said Singapore is trying to grow its pool of family physicians to meet its target of 3,500 by 2030.
Overall, about 200 overseas-trained Singaporean doctors come back every year, he added.
Government will pay for screenings, vaccinations under Healthier SG: Ong Ye Kung
By Joyce Teo, Senior Health Correspondent, The Straits Times, 6 Oct 2022
Singaporeans who sign up to a new national preventive healthcare programme will gain advantages through benefits such as free health screening and the use of MediSave funds to pay for chronic diseases, said Health Minister Ong Ye Kung in a radio interview on Thursday.
Making a pitch for the voluntary programme, which is expected to kick off in the second half of 2023 with those aged 60 and above, he said health screening and vaccinations that are nationally recommended will be paid for by the Government.
Residents who sign up for the Healthier SG initiative will first have to enrol with a primary care doctor, who will develop a health plan and help them manage their care, said Mr Ong in the interview with DJs on radio station One FM 91.3.
"We are asking doctors to set aside capacity for that, so that you have a dedicated doctor-patient relationship with the family doctor," said Mr Ong.
"The doctor may send you for health screenings. That will be free from henceforth," he added.
"You may be sent for vaccinations, nationally recommended ones, namely, influenza, pneumococcal vaccinations, especially for seniors. That will be free."
On Wednesday, Parliament endorsed the White Paper on Healthier SG after a two-day debate.
Mr Ong said one's health plan could include losing some weight, for instance. "Usually, this is not about drug prescription any more. Once you go into preventive healthcare, I'm sure many of you know, you will go into what we call social prescription: your diet, your sleep patterns, your eating habits, your exercise habits, and a doctor should advise you," he said.
"And then we will support the doctor with all kinds of community activities that we're going to organise (and) health screening is critical."
Another important change is that residents on Healthier SG will be able to pay for the care of chronic conditions entirely from their MediSave accounts.
"Some people have chronic diseases like diabetes, so they use their MediSave to manage those diseases. Today, they have to pay 15 per cent cash as co-payment. We always say self-responsibility, we will remove that. So you can use your MediSave fully," said Mr Ong.
Other benefits of the programme include earning points on the Healthy 365 mobile app, which is used for initiatives like the National Steps Challenge.
"When it comes to preventive care, the most important factor is ourselves: what we intend to do differently from before," said Mr Ong, even as he acknowledged the challenges of making changes.
"When I came to MOH (Ministry of Health), then, as I interacted with the folks from the hospitals, from HPB or Health Promotion Board, I found our advice to people to stay healthy is a bit too austere," he said.
"You tell us to be healthy, you cannot eat, no sugar, no salt, everything bland, who would want to lead that kind of life in Singapore, right? So I think it's much better to say we can enjoy our food but in moderation."
"I mean, what's wrong with eating chwee kueh (rice cakes topped with preserved radish) for breakfast, right?" he quipped.
"If you have that in the morning, you can go a bit lighter on the food at lunch, and at night, you can still have your alcohol, like a glass of wine."
Mr Ong said his weakness is watching what he eats but he limits his alcohol to a moderate intake on weekends. He also does pilates or stretching exercises every morning because of a previous back injury.
Asked if Singapore would consider giving mental health days off, he said: "My own sense is that what's more important now is to have flexibility. (Flexible) work arrangements are probably more important because it's always that one hour you need to just run off in the afternoon, get something done for your parents, for the children, or that two hours off, and at night, you work anywhere."
Mental health is an area where the focus should also be more on prevention than on the remedial action, which can be too late sometimes.
"So for mental health, one of the simplest preventive actions is actually not your leave, it's just sleeping enough, letting your brain have a chance to rest and repair itself every night," said Mr Ong.
DJ Glenn Ong asked if Singapore was moving towards the direction of free medical care. In response, Mr Ong said this could not be done.
"Once you make something free, the demand just shoots up and you will get over-prescriptions, you've got people demanding healthcare (when they don't quite need it). Preventive care takes a backseat since curative care is free," he said.
This is why co-payment is always a central feature in the Singapore system, although the Government is now making a small break in its policy for preventive care such as health screenings and vaccinations.
"We make it free because prevention, I think, is important," said Mr Ong.
Healthier SG a decisive shift to get population healthier, keep costs sustainable: Ong Ye Kung
By Salma Khalik, Senior Health Correspondent, The Straits Times, 12 Oct 2022
Singapore has done all it can to reduce the burden posed by chronic illnesses, but the number of people suffering from conditions such as high blood pressure continues to go up, pushing up healthcare costs.
Hence the need to shift the strategy towards greater preventive care, said Health Minister Ong Ye Kung on Wednesday.
Mr Ong said the ministry's new Healthier SG initiative to keep people healthier for longer is an important effort to reverse rising costs, noting: "We will try everything we can to cope with the disease burden."
These have included rigorous evaluations on whether treatments provide value for money, "removing the distortions caused by reckless medical insurance practices", and linking payment with patient outcome.
"It is not too late to shut the dam, and the way that is the most impactful and simplest to understand is to focus on preventive care," Mr Ong told 1,300 healthcare professionals in a keynote address at the Singapore Health and Biomedical Congress at the Singapore Expo.
The National Healthcare Group's (NHG) two-day annual congress theme this year is "reinventing healthcare", with sessions looking at transforming the healthcare workforce and the impact of technology on care.
Mr Ong said one silver lining has been that the prevalence rate for diabetes has remained stable, most likely because of the many measures taken in the country's war on diabetes. But other chronic conditions such as high blood pressure and cholesterol levels are still going up among adults.
Likening the slide into poor health to people on a travellator who do not notice its movement, the minister said what was "scarier" was that most people with deteriorating health are oblivious to the impending danger they are being carried towards.
Alerting people to this danger, such as through the publicity given to the Healthier SG initiative, may prevent them from getting onto the travellator in the first place, he said.
"Clinicians know that preventive steps in our daily lives can fob off severe illnesses later on in life. That is the genesis of our long-term, multi-year healthcare transformation journey, called Healthier SG."
It seeks to empower people to take charge of their own health. More are already opting for healthier drinks he said, noting: "Sales of beverages with less than 5 per cent sugar content have gone up, from 37 per cent in 2017 to 60 per cent in 2021."
The mandatory nutrition labelling by the end of this year for pre-packed drinks will hopefully nudge even more people to pick healthier options.
Physical exercise is critical to better health, and the minister hopes "gamification" will make healthier living more attractive.
The Health Promotion Board's National Steps Challenge, for instance, which gives participants small rewards for achieving their health goals, such as a certain number of steps a day, has shown this works.
People who are in the early stages of chronic diseases - "on the initial part of the travellator and moving slowly" - will be encouraged to change their lifestyles and return to good health. Under Healthier SG, family doctors will be brought on board and older people urged to commit to one doctor.
The ministry will subsidise this move from next year with people 60 years and older, and reduce the eligible age to 40 years in the next few years.
"The physical act of enrolment, committing to build a long-lasting patient-doctor relationship, receiving a health plan with diet adjustments and exercise as 'social prescriptions', will hopefully make the penny drop," he said.
In addition, MOH is working with a network of health, social and community partners to support people to live healthier lives through organised activities.
Mr Ong said such community spaces would be important, citing one in Yishun called Wellness Kampung, which facilitates residents to form their own interest groups, such as social dance, language lessons and qigong.
These peer-led groups help older people stay active and provide a social network, "the most critical prerequisite to stepping off the travellator", said Mr Ong.
Finally, for those who can no longer "step off the travellator", Healthier SG will strengthen integrated care models to improve the care of chronic diseases.
NHG Group chief executive Professor Philip Choo said NHG has identified several major shifts to better care for an ageing society and rising chronic problems. These include a single care plan for each person, regardless of whether he is seeing a specialist, primary care doctor or in hospital. There will be increasing use of data "to gauge how motivations and attitudes influence health behaviour" so interventions can be more targeted, he added.
Looking to the future, Mr Ong said wearable technologies can also play a role in managing chronic diseases, by identifying anomalous readings specific to an individual and prompting them to take follow-up actions.
More will also be done so people can spend their final days of life at home with their loved ones, rather than in a hospital bed.
The authorities aim to lower the proportion of people dying in hospital from 60 per cent now to 50 per cent within the next five years.
While Singapore continues to learn to live with Covid-19, it also has to reimagine and reinvent its healthcare delivery in preparation for a much older population.
Mr Ong said: "Healthier SG is a decisive shift in focus towards preventive care to improve our population's health, reduce disease burden for the long term, reduce suffering of people and put our healthcare system on a more sustainable financial footing."
********************
Related
Opening Speech by Mr Ong Ye Kung, Minister for Health, At the Healthier Sg White Paper Debate 2022, “shaping A Healthier Singapore” - 4 October 2022





No comments:
Post a Comment